
|
|

|
|
| April 24, 2024 |
|
Survey: Who may be at the highest risk for long COVID? 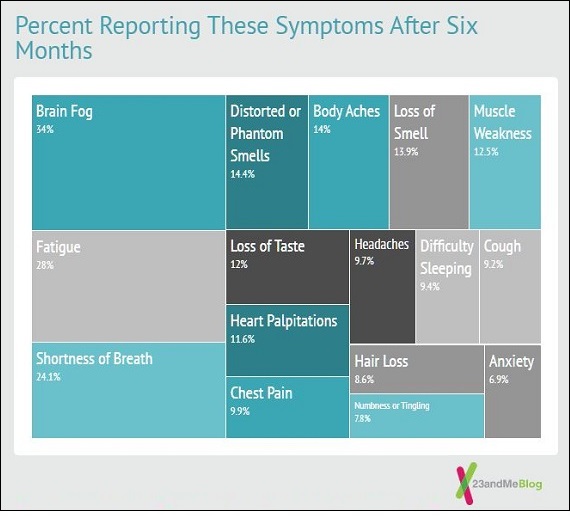
SOUTH SAN FRANCISCO - It's a question everyone wants answered: Who is more likely to develop long COVID-19, the debilitating symptoms that can linger for weeks, months or even longer, after an infection?
A new unpublished study from 23andMe is part of a growing body of research shedding light on who experiences post-COVID conditions and why. The survey, which was voluntary and relied on people self-reporting symptoms, had several major findings, including that women were far more likely to experience long-term symptoms, as were people with a prior diagnosis of depression or anxiety. More than half of people who reported a diagnosis of long COVID had a history of cardiometabolic disease, such as heart attacks or diabetes. The 23andMe survey included 100,000 people who reported a diagnosis of COVID. Of those, 26,000 described experiencing symptoms of COVID at least a month after being infected. In addition, more than 7,000 participants reported an official diagnosis of long COVID. Survey participants were asked about their symptoms at 3, 6 and 12 months. According to Centers for Disease Control and Prevention estimates, about 13.3% of people with COVID will experience symptoms for at least a month, and 2.5% of people will experience symptoms for longer than three months. Dr. Stella Aslibekyan, a genetic epidemiologist for the consumer genetics company, which is based in South San Francisco, told SFGATE that the 23andMe study is unique because it's so large and directly surveyed people about their symptoms. Many other studies into long-term symptoms are smaller, and based on data from medical records, as opposed to self-reported experiences. "We're able to paint a more complete picture of the COVID experience than would be possible from just using medical records," Aslibekyan said. There are limitations to this approach, too. Participating in the study was voluntary, as opposed to a random sample of patients in a health system. The demographics and characteristics of people represented in these kinds of “self-selecting” studies are often skewed, based on who has enough time and interest to fill out the surveys. The study, which has not been peer-reviewed or published in a medical journal, is part of an effort to solve the mystery of why so many people experience symptoms such as shortness of breath, cough, fever, fatigue, brain fog or chest pain for weeks to months after a COVID infection. Many of these symptoms align with the symptoms of chronic fatigue syndrome, a poorly understood condition that has often been linked to other viral infections, including flu and Epstein-Barr. "One hypothesis positions long COVID as an autoimmune condition, in which the immune system is attacking the body's own tissues," Aslibekyan said. Many studies have found that long-term symptoms are much more likely to occur in the most severe COVID cases, but the U.S. Centers for Disease Control and Prevention says that "anyone who was infected with the virus can experience post-COVID conditions, even people who had mild illness or no symptoms from COVID-19." "Researchers found that individuals with COVID who required hospitalization had a more than ten-fold risk of being diagnosed with long COVID compared to those who were not hospitalized when controlling for age, sex, and ethnicity," 23andMe said. Depression and anxiety also seem to be risk factors. To Aslibekyan, one of the most illuminating findings in the survey was that people diagnosed with long COVID were twice as likely to report experiencing depression or anxiety before they were infected. There is extensive research into the relationship between depression and the immune system. People with diseases that cause over-activation of the immune system are more likely to be diagnosed with depression, and vice versa. "When [depressed people] are hit with that acute COVID-19 infection, those long term symptoms also represent inappropriate malfunction of the immune system, so it makes sense that they're more vulnerable to those long-term dysfunctions of the immune system," Aslibekyan said. Women are more likely than men to have long COVID Researchers also found that people with two X chromosomes in each cell were more than twice as likely to report a long COVID diagnosis than those with only one. This finding is consistent with other studies that have found women are less likely to die from COVID, but more likely to develop long-term symptoms. The X chromosome is home to many genes that control immune responses. While most men inherit just one copy from their mothers, women generally inherit two — one from each parent — and, therefore, two sets of those important immune-related genes. (In every individual cell, one or the other X chromosome is switched “on” at random.) That genetic diversity is often a good thing; women are better able to fight off many illnesses than men, for instance. But it’s also linked to a higher rate of autoimmune diseases among women, including multiple sclerosis and Sjogren’s syndrome, Aslibekyan said. Brain fog was the most commonly self-reported symptom The symptom most commonly reported by people responding to the survey was brain fog, a term for sluggish thinking, followed by fatigue, shortness of breath and loss of smell. Among people who received long COVID diagnoses, about 19% reported brain fog a year after infection. Among participants who received vaccines after catching COVID, more than half (55%) reported no change in their symptoms, 25% reported an improvement in symptoms, and about 13% reported that their symptoms got worse. The rest did not know, weren't sure or didn't answer. Story Date: July 22, 2022
|